
Do you have acne, or is it an imposter? How can you tell? Acne is a common skin condition that affects millions of people worldwide. However, there are several conditions that can mimic acne, making it difficult to differentiate between them. In this blog, I’ll walk you through some of the most common acne imposters: folliculitis, keratosis pilaris (KP), and perioral dermatitis.
I’ll outline key identifiers for these conditions along with product solutions that can help clear your skin. Although these “imposters” can look similar to acne, they are quite different and don’t respond to traditional acne treatments.
Folliculitis
Folliculitis is a common skin condition that occurs when hair follicles become infected with bacteria or fungi. It can look similar to acne, but instead of blackheads and whiteheads (comedones), it typically presents as small, red bumps that may be itchy or painful. Folliculitis can occur anywhere on the body where there are hair follicles, but it is most commonly found on the scalp, forehead, jawline, neck, chest, and back.
Common Types of Follicultis:

Bacterial Folliculitis
Bacterial folliculitis is the most common type of folliculitis. It is characterized by a rash of itchy, pus-filled bumps that occurs when hair follicles become infected with bacteria, usually Staphylococcus aureus (staph). Staph bacteria are always present on the skin, but cause issues when they find entry into the body.
At-Home Treatments: Face Reality Acne Med can be helpful with this type of folliculitis to reduce and kill staph infections. After clearing, you can use Face Reality Mandelic Face & Body Scrub as a preventative.

Pseudofolliculitis Barbae (PFB) – (also known as shaving bumps)
Also extremely common, this form of folliculitis comes from ingrown hairs. It occurs when the hair follicle is damaged by friction, shaving, waxing, or tweezing, and is most common in people with curly or coarse hair. When hair tries to grow back, it causes rash, itching, pimples, and pustules that may crust over. PFB most commonly afects those who regularly shave their face but can also happen when shaving the legs or bikini area.
At-Home Treatments: It is recommended to cease shaving for four weeks while clearing PFB. If you must continue shaving, try using an electric shaver, single-edged razor, or a depilatory. For treatment and prevention, use topicals such as Face Reality Mandelic Face & Body Scrub, Rhonda Allison Mandelic Perfecting Polish, or BiON Mandelic Serum (choose 8% for the face or 15% for the body).

Malassezia (Pityrosporum) Folliculitis – (also known as fungal acne)
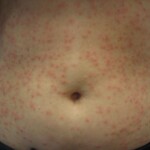
This form of folliculitis is an inflammation of the hair follicle caused by a fungal infection or yeast. Malassezia yeast is always present, but causes issues when there is an overgrowth on the skin. Malassezia folliculitis can appear as small papules or pustules on the skin, often on the chest, back, and upper arms. It can result from extended use of antibiotics or steroids, oily skin, humidity, occlusive clothing, and heavy moisturizers. The condition can be itchy and uncomfortable, and may persist for several months or longer if left untreated.
At-Home Treatments: Treatment options typically involve the use of topical or oral antifungal medications, as well as good skin hygiene practices to prevent the yeast from thriving on the skin. Face Reality Mandelic Face & Body Scrub and Rhonda Allison Mandelic Perfecting Polish are effective antifungals that can be used all over the body for treatment.
Photo: “Pityrosporum folliculitis” from Ran Yuping is licensed under CC Attribution ShareAlike 3.0 Unported
Pseudomonas Folliculitis – (also known as Hot Tub rash)
Pseudomonas folliculitis, or “hot tub” folliculitis, typically occurs after exposure to contaminated bodies of water such as swimming pools, hot tubs, water slides and sometimes even freshwater sources. The pseudomonas bacteria thrives in heated, moving water where chlorine and pH levels are imbalanced. Symptoms of this infection include itchy, red bumps that may be filled with pus and appear within hours to days after exposure.
At-Home Treatments: Pseudomonas folliculitis is usually not a serious infection and can clear up on its own within a week, but in some cases, antibiotics may be necessary to treat the infection. As a prevention, avoid using contaminated water sources and properly clean and maintain swimming pools and hot tubs.
Photo: “Folliculitis” from James Heilman, MD is licensed under CC Attribution ShareAlike 3.0 Unported
Gram-negative Folliculitis
This is another form of bacterial infection that causes red or pus-filled bumps around the mouth and nose area. It often develops in people receiving long-term antibiotic therapy for acne, such as tetracycline or other topicals. The prolonged use of antibiotics leads to the development of antibiotic-resistant bacteria that are difficult to eradicate.
At-Home Treatments: The course of treatment for gram-negative folliculitis typically involves a combination of antibiotics, topical creams, and other prescription medications.
Keratosis Pilaris (KP)

Keratosis pilaris (KP) is a common skin condition affecting millions worldwide. It appears as small, non-inflamed, red or skin-colored bumps that resemble acne and typically develop on the upper arms, thighs, and buttocks. It is often referred to as “chicken skin.” KP occurs when keratin, a protein found in the skin, builds up and plugs hair follicles. The condition is most common in children and adolescents, but can also affect adults. It can worsen in dry winter weather. Although harmless, KP can be very frustrating to treat.
At-Home Treatments: There is no cure for KP, but regular exfoliation and moisturization can help improve the appearance of the affected areas. Begin with a mandelic scrub such as Rhonda Allison Mandelic Perfecting Polish. Treat the area with either FarmHouse Fresh Smooth Reveal Resurfacing Body Serum or BiON Glycolic 20% Skin Cream and nourish with Rhonda Allison Mandelic Replenish or Dr. esthé Dual Barrier Lotion.
Perioral Dermatitis

Perioral dermatitis is a common skin condition that presents as patches of itchy red or tender spots around the mouth, nose, and chin and can even spread up to the eye area. It often looks like small, red, acne-like breakouts and appears dry and flaky. The cause of perioral dermatitis is not fully understood, but it is believed to be related to a disruption of the skin barrier, an overgrowth of bacteria, or a reaction to topical products. Symptoms can be worsened by certain triggers such as harsh cleansers, steroid creams, or oral contraceptives.
At-Home Treatments: Treatment typically involves avoiding triggers, using gentle skincare products, and in some cases, prescription topical or oral medications. Perioral dermatitis can be successfully controlled with proper management but may recur if triggers are not avoided. Other recommendations: Don’t exfoliate or treat with acne products, stop using toothpaste with fluoride or sodium laureth sulfate, limit acidic foods, and don’t use occlusive moisturizers. You can treat using Hale & Hush Quiet Wash and nourish with NeoGenesis Barrier Renewal Cream or Dr. esthé Dual Barrier Lotion.
GENERAL TIPS
- Avoid overly emollient or creamy moisturizers, sunscreens, and oils.
- Keep the affected areas as dry as possible.
- Avoid wearing constrictive clothing or clothing that doesn’t allow the skin to breathe.
- Use a clean washcloth or towel every time you cleanse your skin.
- Avoid sugar and yeast-containing foods (bread, alcohol, processed/frozen foods, deli meat, and dairy).
- Wash clothing and linens regularly and avoid fabric softeners, dryer sheets, and harsh detergents.
- To prevent flare-ups, avoid hot tubs or taking very hot showers or baths.
- If you experience pseudofolliculitis barbae, practice these safe shaving habits:
- Shave less often.
- Wash your skin with warm water and a mild facial cleanser before shaving.
- Use a Lush Cloth or Clean Skin Club Clean Towel in a gentle circular motion to raise embedded hairs before shaving.
- Shave in the direction of hair growth.
- Use a clean, sharp blade and rinse with warm water after each stroke.
- Avoid shaving the same area more than twice.
ANTIFUNGAL SUPPLEMENTS
*If you suspect you have a fungal infection, here is a list of supplements to look for. Select one or two and rotate every few weeks:
.
- Probiotic supplements – These are good if you have been on antibiotics for a long time. No need to rotate as often as other supplements. We recommend HUM Nutrition Skin Squad
- Coconut Oil (or caprylic acid) – taken internally, NOT as a topical product.
- Undecylenic Acid
- Grapefruit Seed Extract
- Olive Leaf Extract
- Neem Oil (topical use only)
- Oil of Oregano
- Apple Cider Vinegar (tablets or liquid)
- Garlic
- Pau D’Arco
- Berberine
- Grape Seed Oil
In conclusion, not all skin conditions that look like acne are actually acne. Folliculitis, keratosis pilaris, and perioral dermatitis are three common acne imposters that can be difficult to differentiate from acne. If you’re unsure about which type you have or how to treat it, reach out to us at AOS. Whether it’s our live chat or a full Acne Coaching program, our knowledgeable team of estheticians is here to answer your questions.

Have questions? Reach out to our team of seasoned estheticians via live chat or sign up for one of our Skincare Coaching Programs to discuss your specific needs. We’ll be here every step of the way!









Comments (2)
Great info!!! I’m an esthetician in California. Can’t wait to hear more from you!
Thanks for the awesome information, I”m a Dermotricologist in New York. Keep putting out this great info.